Schizophrenia May Be Linked to Iron and Myelin Deficits in the Brain, New Neuroimaging Study Reveals
A new neuroimaging study from researchers at King’s College London, Imperial College London, and Hammersmith Hospital has shed light on one of the most puzzling aspects of schizophrenia — the changes that occur in the brain’s structure and chemistry. Published in Molecular Psychiatry in 2025, the research found that people with schizophrenia show reduced levels of iron and myelin in specific brain regions. These findings could help scientists better understand the biological roots of the disorder and pave the way for new diagnostic and treatment strategies.
Understanding Schizophrenia
Schizophrenia is a serious mental health condition that affects how a person thinks, feels, and behaves. It often involves hallucinations, delusions, disorganized thinking, and difficulties in focusing or expressing emotions. Despite decades of research, the exact biological causes of schizophrenia are still unclear.
Researchers have long suspected that schizophrenia may involve structural or chemical abnormalities in the brain. Among the many biological factors under investigation, iron and myelin have recently drawn increasing attention.
- Iron plays an essential role in brain function. It’s involved in energy metabolism, neurotransmitter synthesis (including dopamine), and maintaining healthy neurons. But the brain must keep iron levels carefully balanced — too little impairs normal brain processes, while too much can cause oxidative stress and cellular damage.
- Myelin is the protective sheath that wraps around nerve fibers, allowing for fast and efficient transmission of electrical signals. Damage or loss of myelin can lead to slower neural communication and is thought to contribute to several neurological and psychiatric disorders.
Earlier studies hinted at a link between schizophrenia and abnormalities in both iron and myelin levels, but the results were inconsistent. Some studies showed increased iron, others showed decreases, and many didn’t distinguish between the two factors. This new research attempts to clarify the picture using advanced MRI-based brain imaging techniques.
What the Researchers Did
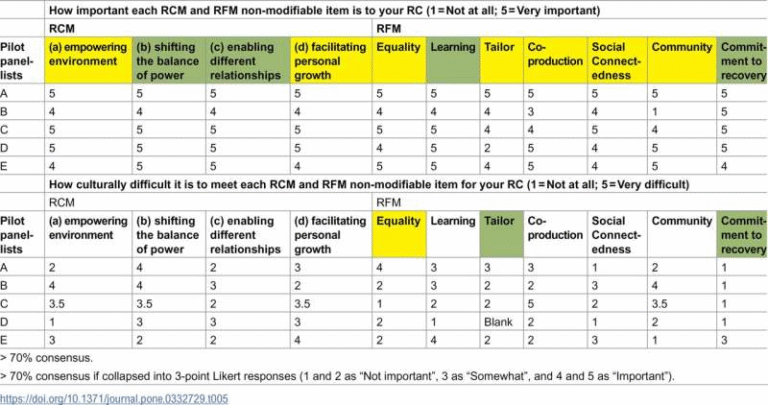
The study included 85 individuals diagnosed with schizophrenia and 86 healthy control participants, matched by age and sex. Participants were between 18 and 45 years old, which helped minimize the influence of age-related changes in brain iron or myelin. People with neurological, endocrine, or substance use disorders (except mild cannabis exposure) were excluded.
The researchers used quantitative susceptibility mapping (QSM) and diffusion tensor imaging (DTI) — two advanced MRI methods that can estimate brain iron and myelin content.
- Magnetic susceptibility (χ): measured using QSM, it increases with iron levels and decreases with myelin.
- Mean diffusivity (MD): derived from DTI, higher MD values usually indicate less myelin or reduced tissue density.
- Magnetic susceptibility anisotropy (δχ): a more specific indicator of myelin in white matter.
By comparing these measurements between the schizophrenia group and healthy controls, the team could infer whether the observed changes were due to iron, myelin, or both.
They focused on key subcortical regions of the brain — including the caudate, putamen, globus pallidus, and substantia nigra/ventral tegmental area (SN-VTA) — areas known to play important roles in motivation, reward processing, and motor function, all of which can be disrupted in schizophrenia.
The Competing Hypotheses
The researchers set out to test two main ideas:
- The Myelin Hypothesis: Lower magnetic susceptibility in schizophrenia could indicate increased myelin, since myelin reduces susceptibility.
- The Iron Loss Hypothesis: Alternatively, lower susceptibility could result from reduced iron levels, independent of or in combination with myelin loss.
To find out which explanation fit the data, they looked at how χ (susceptibility), MD (diffusivity), and δχ (myelin anisotropy) related to each other across brain regions.
What They Found
The results clearly favored the iron loss hypothesis.
- People with schizophrenia showed lower magnetic susceptibility (χ) across several brain regions compared to healthy controls.
- They also had higher mean diffusivity, meaning less myelin density, and lower magnetic susceptibility anisotropy, which also points to reduced myelin.
The affected regions included the caudate, putamen, and globus pallidus, with the largest difference in the globus pallidus. These areas are rich in oligodendrocytes — the brain cells responsible for producing myelin.
When the team looked at gene expression maps from the Allen Human Brain Atlas, they found that the brain regions showing the biggest changes in susceptibility also had high expression of oligodendrocyte-related genes. This strongly suggests that oligodendrocyte dysfunction could be at the center of these changes, linking reduced iron and myelin directly to cellular processes involved in schizophrenia.
Further gene enrichment analyses showed that the regions with reduced iron were also linked to genes involved in glutamatergic signaling, while other regions were associated with genes tied to transmembrane transport and neuronal communication.
Why Iron and Myelin Matter
This study strengthens the idea that iron and myelin are closely interconnected in brain health — and that their disruption could play a major role in psychiatric illness. Oligodendrocytes rely on iron to produce myelin, so when iron levels fall, myelin synthesis can suffer. This, in turn, could slow down neural communication and affect how different brain regions coordinate — a hallmark of schizophrenia’s cognitive and perceptual disturbances.
The researchers also noted that brain susceptibility (χ) tends to increase with age, reflecting normal iron accumulation. However, in schizophrenia, susceptibility was consistently lower even after adjusting for age, suggesting a disease-related process rather than simple aging.
Implications and Next Steps
The findings open new directions for research and potential treatments. If iron and myelin loss contribute to schizophrenia’s symptoms, future therapies might focus on restoring healthy iron levels, promoting myelin repair, or protecting oligodendrocytes.
The team plans to test these same imaging markers in bipolar disorder and in individuals at high risk of developing schizophrenia. They also want to see whether these iron and myelin markers can predict treatment response — for example, whether patients who recover better show more normalized brain iron or myelin over time.
A Few Limitations to Keep in Mind
Like any study, this one has its caveats. It was cross-sectional, so it captures a single moment in time rather than showing how brain iron and myelin change over the course of illness. The participants were mostly in the early stages of schizophrenia, so it’s unclear whether these findings apply to chronic or treatment-resistant cases.
MRI techniques such as QSM and DTI provide indirect measures — they can’t perfectly separate iron from myelin, and their precision depends on model assumptions. Additionally, the correlations with gene expression data rely on postmortem brain atlases, which may not fully reflect living brain function.
Still, the consistency of the imaging and gene expression findings gives this study significant weight. The observed combination of lower iron, reduced myelin, and oligodendrocyte involvement provides a compelling biological framework for understanding schizophrenia beyond traditional neurotransmitter theories.
Broader Context: Iron, Myelin, and Mental Health
These results fit into a growing body of evidence linking white matter changes and iron metabolism to mental health disorders. For instance, reduced myelin integrity has been reported not only in schizophrenia but also in bipolar disorder, major depression, and even autism spectrum disorders. Iron deficiency during development has also been associated with cognitive and emotional difficulties later in life.
Understanding how these biological systems interact could help researchers design interventions that address the root causes of brain dysfunction rather than just managing symptoms.